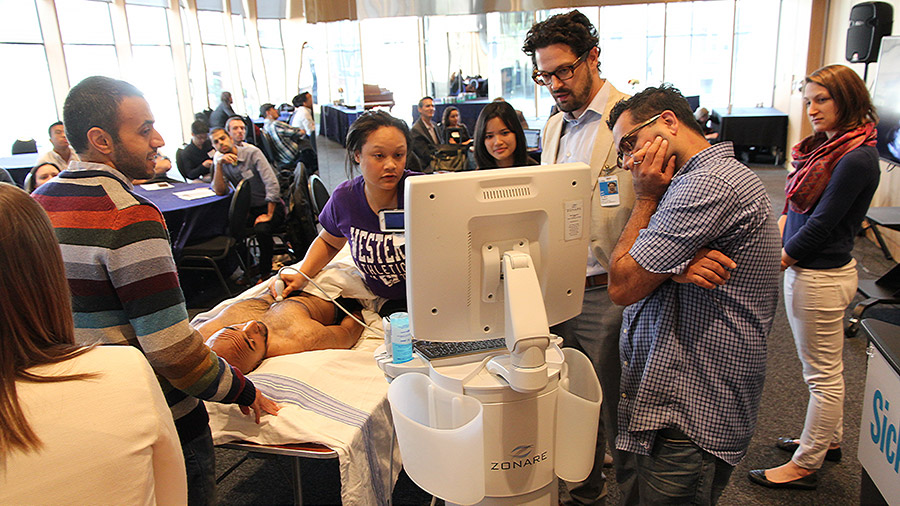
There is no denying that simulation-based training has revolutionized medical education. At U of T Medicine and across our affiliated teaching hospitals, we’re fortunate to have a broad range of simulation centres. We also use simulation extensively in the training we deliver in our MD and post-MD programs. Our learners get the opportunity to practice delicate techniques or complex diagnoses on very highly credible and nuanced models.
In addition, we’re active in SIM-one, a not-for-profit organization connecting the simulation community across Canada and beyond. It includes over 1,700 individuals involved in all levels of healthcare simulation, from a variety of healthcare professions and sectors, including higher education, hospitals, government and industry.
As with any major innovation, though, it’s critical to ensure we’re using it effectively and integrating it successfully into our training programs. A 2011 report by the Association of American Medical Colleges observed that “simulation has the potential to revolutionize health care and address the patient safety issues if appropriately utilized and integrated into the educational and organizational improvement process.”
Simply put, medical simulation-based education is a big, broad world. We need to stay on top of emerging trends and new technology to ensure we’re making optimal use of it. To help us do that, we’ve established a new role — Faculty Lead, Simulation Education Integration — and appointed Professor Doug Campbell to that post. He will work to consolidate, integrate and evaluate simulation education across U of T and our affiliated teaching hospitals.
Professor Campbell is well qualified for this task. An Associate Professor of Pediatrics, he is also the Medical Director of the Allan Waters Family Simulation Centre and Director of Neonatal Intensive Care Unit at St. Michael’s Hospital. In 2012, he was awarded the Marvin Gerstein Award, nominated by the pediatric residents of the University of Toronto for his outstanding teaching. I am very glad he agreed to undertake this important new role.
Supporting him will be the newly established Simulation Education Advisory Committee. It will be chaired by Professor Campbell, with Professor Sal Spadafora, Vice Dean of Post MD Education, serving as Associate Chair. The committee will include representation from the Faculty, simulation centres, affiliated hospitals, the Centre for Faculty Development, SIM-one, and undergraduate and postgraduate learners. The objective is to form a coordinated network to provide advice, promote best practices, identify opportunities for improved collaboration, and increased access to simulation equipment and other resources.
These steps don’t just reflect the significance of simulation-based training, but our commitment to improving and innovating learning at U of T Medicine. Coordinating our activities will not just provide greater efficiencies, but improve the experience for our students and ensure we’re capitalizing on the wealth of opportunities simulation can provide.
Trevor Young
Dean, Faculty of Medicine
Vice-Provost, Relations with Health Care Institutions